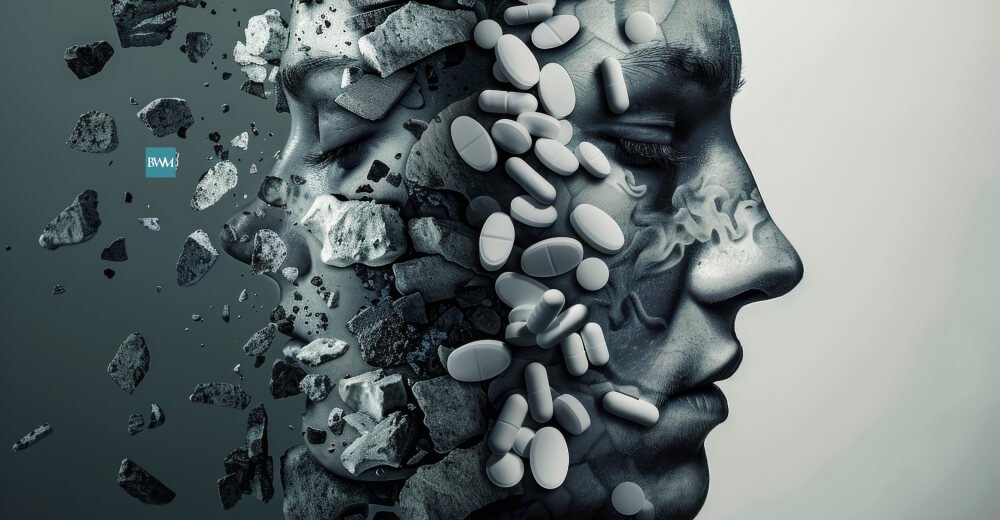
Understanding Dual Diagnosis
Dual diagnosis is where a psychiatric disorder coexists with an addiction. That often creates challenging treatment processes because many psychiatric disorders like depression, anxiety disorder, or PTSD complicate the recovery from an addiction and vice versa.
According to the National Institute on Drug Abuse, 45% of those diagnosed with addiction also have a mental disorder; hence, effective treatment for such dual diagnosis calls for integration and holistic approaches to treatment where dual mental disorders and addiction are treated at the same time for a sustainable recovery.
The Relationship Between Mental Health and Addiction
Mental health disorders often come hand in hand with substance abuse. In fact, many patients suffering from mental health conditions resort to self-medication with drugs or alcohol as a symptom suppressor, for example, stress, anxiety, or depression. A patient suffering from social anxiety disorder will likely find himself or herself drinking alcohol as something that brings comfort in social situations.
On the other hand, substance use could trigger or worsen mental health conditions. Prolonged alcohol or drug abuse alters the chemistry of the brain in a way that leads to mood disorders, psychosis, or impairments of cognitive functions.
Challenges in Treating Co-occurring Disorders
Treating a patient with a dual diagnosis is pretty complex because the two disorders influence each other. If the other disorder remains untreated, it will trigger the relapse of the other one. Traditional addiction treatment models that focus on substance abuse without addressing underlying mental health issues do not bring long-term fruits for those with co-occurring disorders. For instance, when an addict undergoes treatment for one condition and for depression alone, then there is a high likelihood of relapse because such a client would be fighting depressive attacks after recovery.
In addition, the co-occurrence of disorders will usually lead to more severe symptoms and greater functional impairments than when one disorder is present. Such exacerbations ensure that the person has poorer overall health outcomes. Thus, integrated care must be implemented simultaneously, treating mental health disorders and addiction at the same time.
Integrated Treatment Approaches
Effective treatment of dual diagnosis requires an integrated approach, treating mental health and substance use disorders simultaneously through a combination of therapies and, medications and support services. Some important components of integrated treatment are:
• Cognitive Behavioral Therapy (CBT): It will teach how patients can recognize and deal with negative thought patterns and behaviors about addiction, as well as any mental health disorder. This form of therapy builds the strength to cope when exposed to stressors, cravings, or other emotionally triggering aspects.
• Medication-Assisted Treatment (MAT): In some dual-diagnosis patients, treatment involving both of their medical conditions at one time through the use of a variety of drugs may be necessary. For example, though antidepressants are aimed at curing depression, buprenorphine or naltrexone can be used for the suppression of cravings in the case of opioid addiction.
• Peer Support Groups: Group therapy or 12-step programs such as Dual Recovery Anonymous provide an atmosphere of shared experiences and emotional support to people with the dual conditions, both mental illness and addiction.
• Holistic Therapies: Mindfulness, yoga, or even art therapy can help the patient with the emotional and psychological condition of dual diagnosis while keeping him relaxed and self-aware without using substances.
Early Intervention and Comprehensive Screening
Early diagnosis of comorbid disorders is also necessary in effective treatment. Comprehensive mental health and substance use assessments in the initial phases of treatment allow the discovery and treatment of both disorders as early as possible. This is more relevant in primary care, where it is possible to enter primary care with presentations of depression, anxiety, or even other mental conditions without proper assessment of substance use issues.
SAMHSA would encourage these integrated screening tools for substance abuse and mental health. This assessment can help clinicians formulate better, more personalized treatment plans.
The Importance of Long-Term Care and Relapse Prevention
Given this dual diagnosis complexity, treatment must be long-term and continuous. Recovery cannot be linear for these patients, and those with co-occurring disorders do have a greater risk of relapse.
For that reason, any type of support provided immediately upon leaving treatment, including outpatient therapy, aftercare programs, or constant peer support, can ensure that patients remain sober and in control over their mental health.
This makes the treatment plan broader than just psychotherapy because, in addition to it, the strategies to combat relapse should be enhancing stress management, triggers identification, and lifestyle changes that may reduce the likelihood of an individual encountering that stressor and undergoing relapse.
Conclusion
Treatment of dual diagnosis should always focus on balancing the treatment between the addiction and mental disorder. Among other therapies, medications, and support services that are specifically suited to the unique needs of individuals with co-occurring disorders must be included for treatment. This method therefore provides a bigger chance for long-term recovery, reduced relapse rate, and eventually improvement in the quality of life for the individual. In tandem with increased awareness about mental health, there has to be the same awareness and treatment of dual diagnosis among the people so that those with co-occurring disorders are treated for meaningful recovery.